Organizations today are never still. The chances are that your strategy is constantly requiring adjustment, and occasionally a bigger overhaul. Learn how (not) to implement change management in healthcare.
Just in case leaders and others still believe in Change Management as a relevant strategy in healthcare, the following is my perspective on its value and an insight into the alternative.
What is a Change Management Strategy?
When change is required within a function or part of the organization, the next big decision is how to go about doing it. Often this decision is missed because leaders don’t always know that they have a choice — a critically important choice that has enduring and significant consequences.
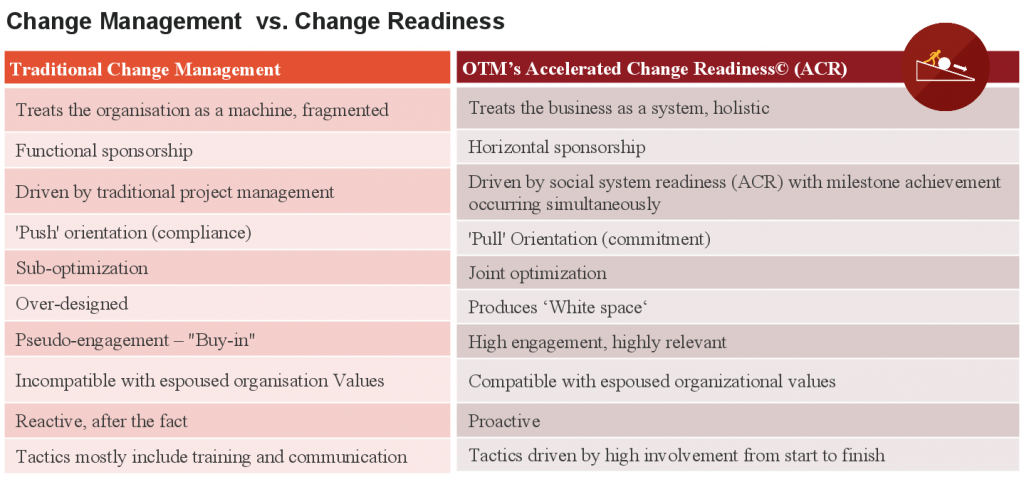
Change management often becomes the default to help with the change process. It is still a widely held belief that it is an effective way to implement change. Change Management is a solution based on ‘after-the-fact’ previous key decisions taken about the change. These have already been taken in isolation from the bulk of the workforce and stakeholders and the problem then becomes one of how to get these changes implemented, to deliver remedial and compliance-driven change.
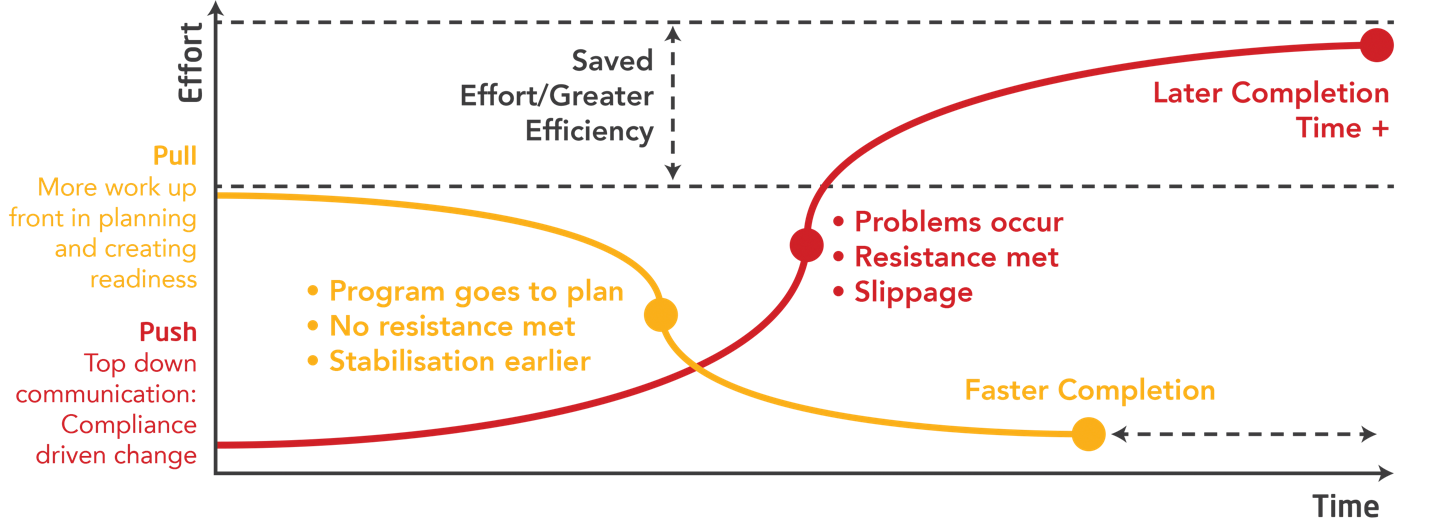
This can often take the shape of leveraging one-way communications, training, and appointment of ‘change champions’, for example. The goal is to generate “buy-in”. What “buy-in” really means is that the change has already been decided, so it becomes about telling the workforce until they comply. We call this “pushing” change onto the business.
As we know, the principles, policy, and provision of healthcare worldwide vary enormously. From the NHS model in the UK (free at the point to delivery) to the highly commoditized version in the USA with all variations in between across different countries. However, one thing is clear that costs continue to increase with the aging populations (we are living longer) and advances in treatments and healthcare. There is a clear need to manage this in a way that both improves the health of our populations, decreases their need for healthcare, and improves quality and manages cost.
Over the last three decades, we have seen the development of a ‘Collaboratives’ movement in healthcare worldwide. The basic premise is the acknowledgment that to affect any positive change at the level of a disease process or the health of a population, those affected have to be involved in making decisions about the things that are going to affect them going forward – positively or negatively. This includes the workforce, stakeholders, patients, and community members. They are involved in making the key decisions about what needs to change and make decisions about how those changes are implemented.
To affect any positive change at the level of a disease process or the health of a population, those affected have to be involved in making decisions about the things that are going to affect them going forward – positively or negatively.
Knowing this, I would be rather surprised if this change management strategy isn’t followed elsewhere in healthcare settings.
Push vs. Pull Approach to Change Management
To achieve a real, sustainable change in healthcare management demands a very different approach. It requires a shift from “managing” change to creating the conditions for change, engaging those affected to take part in the change itself. People are passionate about their work, particularly in healthcare. They want to make a real difference and giving them genuine opportunities to participate in change is when real change happens – when real commitment occurs. We call this “pull”.
The evidence would suggest that Change Management in healthcare is not only outdated and ineffective, it should be dead!
Organizations don’t Change, People Do!
Organizations are made up of individuals and each of us is highly variable. To change anything about the design of a system means that the people who operate in those systems have their daily patterns disturbed. This means change for them and unless they have input and some control over those decisions, their normal and default system is to resist. To alter this state, people must have the opportunity to own the change.
How to Manage Change in Healthcare
For change to be effective in a system, it has to occur at the level of the technical and the social system, simultaneously. The image below helps describe this. In short, for change to really work – the design of the change process has to attend to these in tandem, throughout the process.

Our approach to change is built on the deeply held belief that “people support what they help create”. We use ‘pull’ versus ‘push’ to achieve the most effective outcome; a method that takes a disciplined, step-by-step approach focused on both changing the social system and technical systems at the same time. It ensures that key and impacted stakeholders are ready for change, with a clear understanding of their role and how they can influence lead. It is the delta between Change Management and Change Readiness.
Implementing a Change Management Process in Healthcare
It’s a “Pay Now vs. Pay Later” Decision
In summary, look at it as push versus pull or compliance-based versus commitment-based change. The former will get you speed up-front, poorer quality solutions, significantly more effort, slower implementation complete with starts/stops and pain. Alternatively, invest all of those resources into asking your own people to use their collective brilliance to solve real business issues. Create the space for them to do it. Provide them the resources to support their efforts and get out of the way.
Creating pull for change management in healthcare has to be deliberately planned for and carefully managed and monitored, it does not follow a prescribed timeline but can be accelerated if the conditions are set right. Pull comes from people who have a truly positive perception of the way work is being structured in the future, and of the roles that have been designed to do the work.
Pull does not come from telling people about change through carefully planned and orchestrated communication campaigns and showing them how to do it through brilliantly designed training and development programs. It comes from people who have been involved in determining how their work will be done. To do this they need to have an understanding of where their work fits into the wider value stream of the whole organization. People really do own what they help create.
This is at the heart of our work and also what the Collaboratives movement is trying to create in their setting. The healthcare ‘industry’ is enormous and at a clinical and public health level, all interventions should be evidence-based. It seems bewildering that this principle should not apply to change more widely in this setting and I would certainly strongly advocate against using the retrospective and retrograde approach called Change Management.
Wilma Paxton Doherty is a Consultant at ON THE MARK. OTM’s experience and passion for collaborative business transformation supported by pragmatism, systems thinking, and a belief in people is unparalleled. OTM has been in business for 28 years and is a global leader in collaborative organization design.
We understand that you may want more information on how OTM works with clients, our terms, and further information from our extensive case-study library. Contact us about careers, more information, or how we work here.